
Gum Disease Treatment in New York City
Periodontal Disease Prevention & Treatment
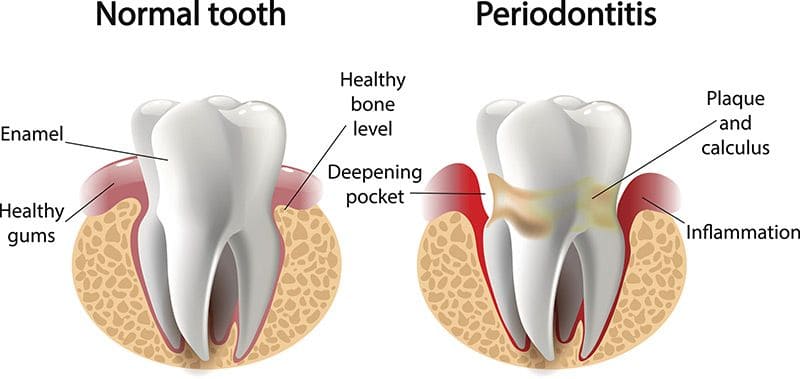
Periodontal disease, also referred to as gum disease, is a chronic bacterial infection of gum tissue that surrounds one or more teeth. Infected tissue is the result of bacterial inflammation caused by plaque. While the biofilm is naturally produced in the mouth, it traps bacteria at its location and can affect the health of the teeth and gums.
If left untreated, periodontal disease can lead to serious issues like tooth loss. Marc Lazare, D.D.S., M.A.G.D. specializes in preventive dental care and everything involved in creating a strong, healthy foundation for your teeth and gums.
Gingivitis
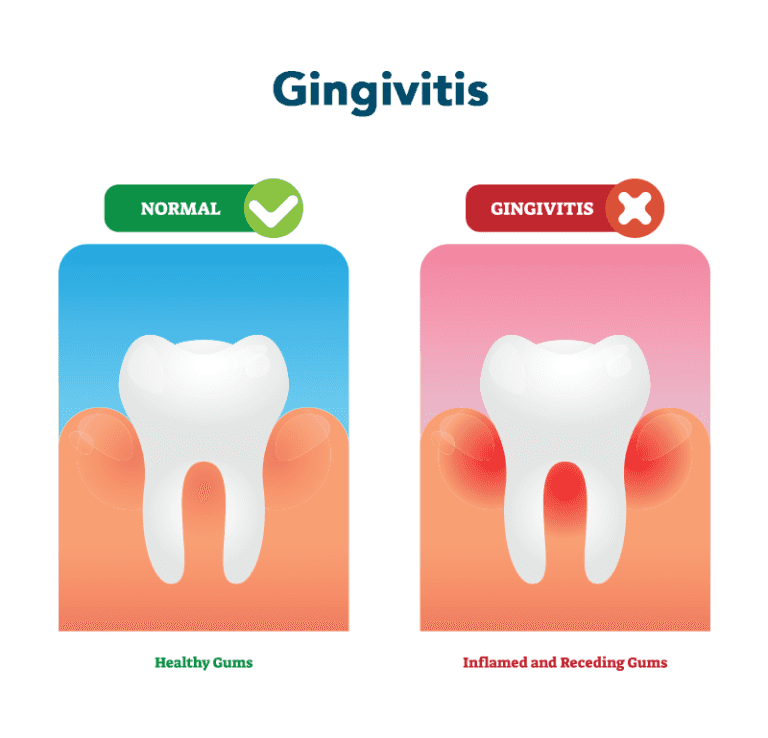
Gingivitis is one example of periodontal disease, though its side effects (tender and reddened gums) are generally mild and reversible with proper care. The diagnostic term gingivitis stems from the word gingiva, which is the medical term for the gums, and the suffix it is, which describes an inflammation.
As plaque hardens or becomes calcified, it transforms into tartar (or calculus). Tartar is typically present at the base of the gums or below the gum line and may build into a thick layer, creating recession of gum tissue, and sometimes a pocket of space between the gums and teeth.
Bacteria of the mouth can become lodged in this area, leading to periodontitis, which is a more serious condition that must be treated by a periodontist. In advanced cases of periodontitis, gum recession leads to the destruction of area bone and the periodontal ligament that supports the tooth.
What is a Periodontist?
A periodontist is a gum specialist who practices advanced dentistry to prevent disease from occurring and utilizes the latest scientific advancements to diagnose and treat periodontal disease. Dentists, like Dr. Lazare, may notice disease progression during a dental exam and will refer the patient to a periodontist. Periodontal specialists not only attended dental school but were also educated during three years of additional schooling at the doctoral level in order to care for gum disease. In serious cases where tooth loss cannot be prevented, a periodontist serves as an expert at placing dental implants to restore regular tooth function, a healthy bite, and good oral health. For this reason, most periodontists have special skills in cosmetic dentistry.
How Is Periodontal Disease Prevented?

Good oral hygiene, including the use of fluoride toothpaste, and regular dental care are the best ways to prevent periodontal disease from occurring in the gums.
Dr. Lazare recommends that patients use a toothbrush with soft bristles and to replace the toothbrush (or in the case of the electric version, toothbrush head) to allow for proper twice-daily cleanings.
The use of oral irrigators and pre-brush rinses like Plax also aid in deep cleanings. As always, regular flossing or the use of interproximal toothbrushes or cleaners is important to remove plaque in between the teeth.
Tongue scrapers offer a great solution for a total mouth cleaning, as the tongue is like a sponge that collects bacteria that can be redistributed to the teeth.
Can Patients Who Have Neglected Their Oral Health for Years Reverse the Damage to Their Mouths?
Unfortunately, irreversible damage in these cases is likely because gum disease leads to receding gums and bone loss, which in turn will not properly support the teeth. Certain patients may qualify for grafting procedures that restore this tissue loss. An STM treatment and at-home care can prevent further damage following a restoration procedure. Broken teeth and tooth decay can be replaced through dental implants and bridges, which will appear natural amongst patients’ other teeth.
Treating Periodontal Disease

 When a patient notices changes taking place in the gums or is informed by dental staff that they could benefit from professional intervention, they may be a candidate for Dr. Lazare’s soft tissue management program. The soft tissue management (STM) program is a non-surgical method of treating and preventing the progression of periodontal disease. It consists of periodontal debridement, or the removal of plaque tartar below the gum line.
When a patient notices changes taking place in the gums or is informed by dental staff that they could benefit from professional intervention, they may be a candidate for Dr. Lazare’s soft tissue management program. The soft tissue management (STM) program is a non-surgical method of treating and preventing the progression of periodontal disease. It consists of periodontal debridement, or the removal of plaque tartar below the gum line.
During the procedure, Dr. Lazare operates a piezo ultrasonic scaler, which is a gentle instrument that utilizes water and ultrasound waves to eliminate calculus deposits from teeth. Scaling and root planing address the health of the periodontium, including the root of the tooth, to remove all buildup and disinfect the area. This process will reestablish the attachment of the teeth to the gums. The irrigation process also utilizes chlorhexidine and fluoride to promote area healing. These medications can be warmed, and anesthesia can be administered for a more comfortable experience.
Patients may be asked to follow up with at-home care consisting of a specific regimen. Dr. Lazare may suggest the use of an electric toothbrush, a special fluoride toothpaste like Prevident, and Perioguard mouthwash. By undergoing the minimally invasive STM treatment and practicing good oral hygiene, patients can avoid tooth extraction and the placement of dental implants or other periodontal surgery. Patients may also be required to schedule more frequent visits with their general dentist for cleanings.
Other Complications of Periodontal Disease
The vast majority of the population – about 75% – is currently experiencing some form of periodontal disease. Studies have shown that this type of inflammation is linked to serious health issues like heart attacks, strokes, diabetes, respiratory diseases, and low birth weight in babies whose mothers are affected. Researchers have found that the type of bacteria in plaque is also present in blood vessels of patients with coronary artery disease. Those with periodontal disease are predisposed to suffer a heart attack as a fatal event and have a higher risk of stroke.
Certain habits like smoking or chewing tobacco have also been connected with gum disease. Some early signs of periodontal disease are bleeding gums when brushing the teeth and continuously swollen, red gums. As it progresses, patients will notice loose teeth with dark spaces between them, and pocketing of 4mm or greater when measured by a dental hygienist.
Routine prophylactic cleanings are designed to protect against gingivitis and periodontal disease. Once inflammation and recession of gum tissue is noted, a patient’s dentist or hygienist will measure gum recession and the gaps between teeth and the surrounding gums in order to follow any disease progression. If the disease cannot be reversed, the dentist will then recommend that the patient schedule an appointment with a periodontist.
Heart Disease & Gum Disease
If a specialist were to tell you that your cholesterol is too high and, as a result, double your chances of developing heart disease, would you kick yourself into action and do something about it?
Most rational people would. In fact, after hearing those words, many would consult a nutritionist, start an exercise regimen, or alter their diet by eliminating cheese or switching to egg whites.
Now, suppose you hear the news that heart disease was twice as high in people with gum disease (or periodontal disease) and you were one of those many people who suffered from this condition.
Would you set up an appointment with your dentist with the same urgency as before?
Studies About the Link Between Gum & Heart Disease
According to some studies, periodontal disease has proven to be among the strongest risk factors linked to heart disease, along with hypertension. Oral bacteria can infect damaged hearts and certain types can cause platelets to aggregate. New findings have emerged explaining how and why gum-disease-causing bacteria can also increase the risk of heart disease. Researchers at Harvard’s School of Dental Medicine and presenters at the 150th annual meeting of the American Association for the Advancement of Science also concluded that the bacteria found in plaque (the primary etiological factor causing gum disease) is linked to coronary disease.
How Does Gum Disease Affect the Heart?
People afflicted by gum disease are twice as likely to suffer a fatal heart attack and nearly three times more likely to suffer a stroke than those with no periodontal issues. It is long thought that oral bacteria, the most well-known kind being streptococci, invades the blood circulation through small ulcers in the gum tissue. The bacteria cause platelets in the circulatory system to build up and create blood clots (known as thrombi) which can block veins and taint heart valves.
At the point when you reflect on the impact of gum disease, think not just as far as how it affects your dental health, but also how it could provoke dangerous and possibly lethal infection from the spread of bacteria into your bloodstream. Avoiding other risk factors like smoking and chewing tobacco which have a detrimental effect on the severity of gum disease is also very beneficial to both gum & heart well-being. Systemic diseases like diabetes can lower the oral tissue’s resistance to infection, making gum disease even more severe.
How to Prevent Gum & Heart Disease
Have your dentist review your medical history in-depth during your appointment. Oftentimes, high cholesterol wouldn’t be the only red flag that can be raised. A considerable lot of the meds or drugs that you might take can diminish your salivary flow and immensely affect your teeth and gums. Prevention and early detection are vital parts in beating heart disease.
The following are symptoms of gum disease:
- Gums that tend to bleed easier and often
- Tender or swollen gums
- Halitosis (bad breath)
- Loose teeth, or teeth that feel like they move
- Secretions between gums and teeth
Infections like gingivitis and more also pose a threat and are considered red flags in such cases. If you suffer from any of the aforementioned signs, contact a professional dentist or periodontist for a thorough diagnosis and treatment plan.
Available Treatments for Gum Disease
There are many procedures, routine check-ups, and other dental & oral services that can aid in the prevention of developing heart disease due to poor oral and dental hygiene. Treatments like periodontics and dental cleanings are necessary to keep gum health steady and minimize your risk of coronary illness. However, there is a wide array of solutions you and your dental specialist can discuss during a consultation or appointment. Teeth are intended to last you a lifetime, and a healthy heart and body should help improve your overall quality of life. They shouldn’t impede one another.


Frequent Gum Disease Questions
-
Can Vitamins and Minerals Really Help to Prevent Periodontal Disease?Absolutely. A lack of certain nutrients can become a factor in periodontal disease by making it more difficult for the mouth to resist infection. Periodontal disease is a condition where the infected gums gradually pull away from the teeth, deepening the surrounding pockets, allowing the infection to destroy the supporting bone. This results in the loosening of the teeth and their eventual loss if left untreated.
Vitamins and minerals play a crucial part in helping the body combat bleeding and swollen gums, loosening of teeth, decay and bad breath. More specifically, vitamins and minerals help to form antibodies, help fight bacteria and infection and aid in the response of the immune system. So what recommendations should a dentist make to his or her patients regarding diet and nutrition? The first suggestion should be to eat a well balanced diet and take the necessary nutritional supplements. Keep in mind that food storage, food processing, freezing and thawing, and cooking depletes the majority of nutrients from foods that were originally nutritious.
There are many other factors that affect the way vitamins and minerals are absorbed into our system. Stress, smoking, alcohol, drugs (pharmaceutical and recreational), pollution and various medical conditions can act to prevent one from receiving the benefits of a well-balanced meal. Remember that disease tends to occur less frequently in a healthy, well-balanced body. -
Can Periodontal Disease Be Hereditary?Yes, gum health can be affected by a person’s genetics, and studies have proven that about one-third of the population is predisposed to periodontal conditions. Even with good brushing and flossing habits, people with inherited oral health issues can be up to six times more susceptible to periodontal disease. Genetic tests can prove this link and heighten the awareness of disease, which can then be proactively prevented.
-
What Are the Different Forms of Periodontitis?There are many different inflammatory bacterial diseases of the gums, but the most commonly found conditions include acute periodontitis, chronic periodontitis, periodontitis as the result of systemic diseases, and necrotizing periodontal disease.
• Acute periodontitis occurs in healthy patients who exhibit the rapid loss of tooth to gum attachment, and subsequently experience the destruction of related bone.
• Chronic periodontitis causes inflammation in the surrounding structures of the teeth that provide support, compromising the condition of attachment, teeth, and bone, albeit progressively. This form of periodontitis is most common and specifically produces recession of the gums and pockets that form between the gums and teeth. Chronic periodontitis is more common in adults.
Gum disease that occurs as the result of a systemic disease can present early in a person’s life. As previously mentioned, common conditions linked to periodontal disease include heart disease, respiratory disease, and diabetes. Lesions of necrotic tissue are characteristic of necrotizing periodontal disease. The infection causes tissue death in the gums, alveolar bone, and periodontal ligament. This form of periodontitis can be seen in patients with immunosuppression or those with compromised immune systems due to HIV or malnutrition. -
What Are the Signs of Periodontal Disease?Periodontal disease often develops progressively and unknowingly due to the absence of pain, but in other cases it can develop rapidly. Unless a patient sees his or her dentist for regular checkups, s/he may not recognize the development of periodontal disease until the gums and bone have been damaged to the point of tooth loss. In other cases, there may be obvious changes to a person’s oral health that can signal an issue such as the following:
• Red, painful gums that are sensitive to brushing and flossing or hard foods
• Gum recession that creates the illusion of longer teeth
• Pus and sores
• Bad breath
• Loose teeth or a change in the fit of partial dentures or regular bite
Periodontal disease can occur at any age, and over half of all people over age 18 show signs of at least the early stages of some form of periodontal disease.
-
Dr. Lazare saved me from getting several crowns and instead he restored my teeth with biomimetic fillings and saved my natural teeth, they look beautiful.
- Ann
Periodontal Examination
During the initial visit to Dr. Lazare’s office, the periodontist will go over the patient’s medical and dental history, including current medications they may be taking. Next, the patient undergoes an examination of oral and periodontal health. The periodontist will assess recession of the gums and perform measurements of associated periodontal pockets, survey the bite, and determine if any of the teeth have loosened. It may be necessary to perform imaging of the mouth (x-rays) to view potential bone loss between the teeth.
Patients with diabetes should inform their oral health providers of their condition. The best time to be in the chair is about 90 minutes after a diabetic patient has eaten and taken their diabetes medications. A more condensed morning visit tends to work well. Diabetic patients should also ensure they are scheduling exams twice a year.
Contact the office at (332) 334-8290.

to Get Started? Call Us at 332-334-8290 or Schedule Your Next Visit
-
Monday: 8am - 5pm
-
Tuesday: 8am - 5pm
-
Wednesday: 10am - 7pm
-
Thursday: 8am - 5pm
-
Friday: 8am - 5pm
-
Saturday: 9am - 6pm
-
Sunday: Closed

